The measurement depth of LBF is a function of the distance between the incident point and receiving point. The detected laser light intensity, Id, is expressed as,
Id = η・Io・exp ( -γ・L ),
When the tissue is highly scattering material and the Beer-Lambert law is applied.
Here,
η : the coefficient depended on the optical system,
Io : the incident laser light intensity,
γ : the attenuation coefficient of the tissue, and
L : the length the laser light passes.
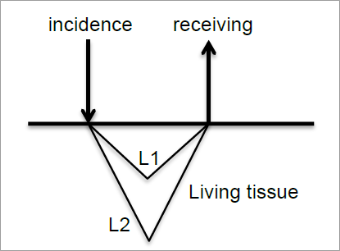
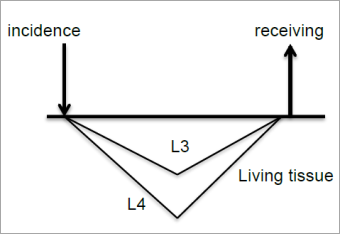
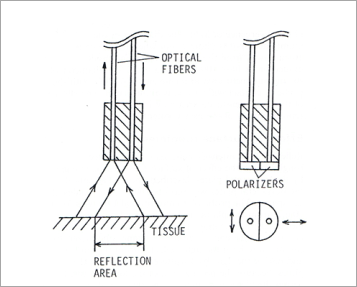
When the distance between the incidence and receiving point becomes longer, the total detected light intensity becomes weaker, but the measurement depth becomes deeper. The reason is that the difference of the detected light intensity between from shallow part and from deeper part becomes smaller when the distance becomes longer. Fig.5 and 6 show the state. Fig. 5 is for the distance is short, and Fig. 6 is for long.
The passage lengths of the light returned from the same depth in the two figures are L1 and L3, and L2 and L4. The light intensity passed through L1 is much stronger than that through L2 because L2 >> L1 in Fig. 5. Therefore, the ratio of the light intensity through L1 is dominant in the total detected light intensity. However, L3 is not so short compared with L4 in Fig.6, therefore, the ratio of the light intensity through L4 relatively becomes lager in the total detected light intensity.
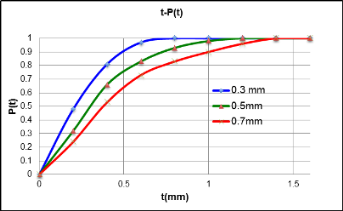
The graph, Fig. 7 shows the result of a model experiment by using polyacetal sheets. The polyacetal sheet has almost the same optical characteristic as human skin1). The distance between the incident and receiving points was set as 0.3, 0.5 and 0.7 mm, and the detected light intensity was measured by piling the 0.2 mm polyacetal sheets. The X-axis is the thickness, t, of the piled sheets, and the Y-axis is the cumulative probability, P(t), normalized by the maximum intensity. This characteristic depends on the divergence of the incident light and the receiving device. In this case, 100 µm optical fibers were used for the incidence and receiving.
This graph shows that the longer distance between the incidence and receiving includes the blood flow signal from deeper part more. Also, it is not easy to decide the maximum measurement depth, like OO mm. For example, when the distance between the incidence and receiving is 0.5 mm, the blood flow signal to 0.8 mm depth occupies 90 % of the total blood flow measurement and, furthermore, the blood flow signal to about 1 mm depth can be detected. The regression analysis indicates that the measurement depth which occupies 95 % of the total blood flow signal is 1.55 X d + 0.12, R2 = 0.999. Here, d is the distance between the incidence and receiving.